Ethics play an important role in healthcare policymaking. It guides the legislator in developing or improving policies based on four philosophical principles: Respect for autonomy, justice, beneficence and nonmaleficence (Longest, 2010). Since Antibiotic Resistance have been a growing worldwide issue, the need for policymakers to include ethical considerations is imperative for them to create a law that would benefit the vulnerable population especially long term care facility residents. Let me discuss to you the following ethical principles that Longest (2010) emphasized which are needed in policymaking:
- The principle of respecting the peoples’ autonomy in policymaking is necessary because it gives them the chance to decide based on their own wellbeing. This makes it ethically appropriate as policymakers must ensure the people that the policy was made is truthful and beneficial to all parties.
- It is important to consider justice in creating policies focused on healthcare delivery. It is the right of every person to have access to healthcare however, policymakers have to critically think on what a fair distribution of healthcare is. According to Longest (2010), justice has three most prominent views on justice that policymakers must reflect on:
- Egalitarian – this means that each person must have equal access to healthcare assistance and inconveniences and that justice should be acknowledged in various levels of need. In other words, more benefits or burdens are given to those people who are sicker, extremes of age, poor, homeless etc. since they are vulnerable with diseases.
- Libertarian – entails a maximum of social and economic freedom for the people which limit governmental interference in distributing healthcare.
- Utilitarian – involves creating healthcare policies for the greatest good of all
- Policymakers who follow the principle of beneficence render choices based on the utmost gain to society as a whole and balance it with the problems of their decisions objectively.
- Lastly, policymakers who are driven by the principle of nonmaleficence generate decisions that lessen injury and to safeguard the quality of healthcare given to the society.
Senator Sherrod Brown from Ohio created a bill that focuses on antibiotic resistance which has now been introduced in the Senate last July 29, 2019. The Strategies to Address Antibiotic Resistance Act or the STAAR Act increases This bill expands numerous proposals to address antibiotic resistance. It also reinstates the interagency Antimicrobial Resistance Task Force to organize and foster attempts to concentrate on antibiotic resistance. Moreover, this bill requires the Department of Health and Human Services to urge health care facilities in executing antimicrobial stewardship programs to appraise and amend the utilization of antimicrobial drugs. On the other hand, this bill also involves the Centers for Disease Control and Prevention (CDC) to utilize the National Healthcare Safety Network to gather and report data about the usage of antibiotic drugs, changes in resistance to such drugs, and other trends influencing patient outcomes. Additionally, the bill increases nationwide efforts to monitor, research, and prevent the spread of infection from resistant organisms (Brown, 2019).
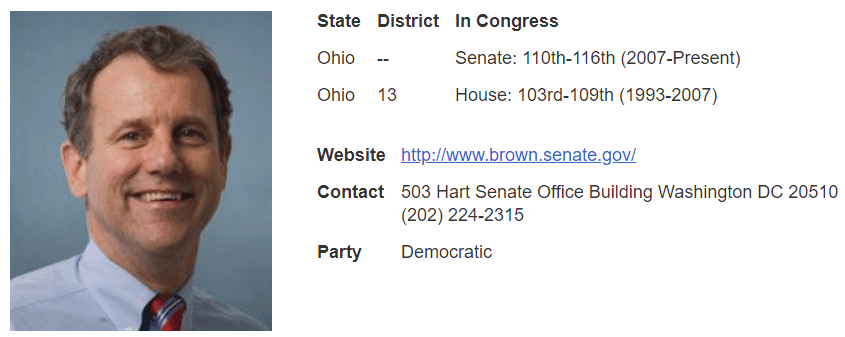
The STARR bill by Senator Brown (2019) was carefully thought out as it considered all four ethical principles in policymaking. It emphasized autonomy as it respects the freedom of the people to know the benefits of Antibiotic resistance and the burden it may cause if not followed. Moreover, justice was highlighted because it showed how antibiotic resistance may affect the those who are considered vulnerable population (elderly in long term care facilities) and the need for initiatives to promote Antibiotic Stewardship should not only be focused on this population but for everyone in the society. Beneficence and nonmaleficence were also accentuated because it promotes goodness and prevent harm to the society by entrusting organizations like the CDC and other government agencies to advocate for better Antibiotic stewardship programs in the United States. Therefore, developing ways to improve antibiotic prescribing in healthcare facilities particularly in those who house vulnerable population like long term care facility residents to counteract antibiotic resistance should be implemented taking into account the ethics behind policymaking.
References
Brown, S. (2019). S.2304 – Strategies to Address Antibiotic Resistance Act. Retrieved from https://www.congress.gov/bill/116th-congress/senate-bill/2304?q=%7B%22search%22%3A%5B%22antibiotic%22%5D%7D&r=3&s=1
Longest, B.B. Jr. (2010). Health policymaking in the United States (5th ed.). Chicago, IL: Health Administration Press.

Crlavelasquez,
I thoroughly enjoyed reading your blog post, and your example of Senator Brown’s bill is an excellent example of the role that ethics may play in healthcare policy-making related to your topic of antibiotic stewardship in long term care facilities. I believe that the ethical principle of nonmaleficence is particularly pertinent to your topic, because healthcare policy would be aimed at reducing unnecessary antibiotic prescribing and therefore the harm that may be associated with this issue.
According to the CDC (2017), “any action taken to improve antibiotic use is expected to reduce adverse events, prevent emergence of resistance, and lead to better outcomes for residents in this [nursing home] setting”. Additionally, taking action through healthcare policy and practice change in order to improve antibiotic use is recognized by this federal organization as a core element of antibiotic stewardship in the long term care setting. Interventions that may contribute to this goal are ensuring the implementation of policies which support optimal antibiotic use; antibiotic “time-outs” which allow clinicians to reassess the indication for antibiotics and the current regimen; integrating pharmacists into the decision-making team; and situation-specific interventions in order to avoid unnecessary prescribing (CDC, 2017).
Overall, the goals outlined by the CDC above, and your goal in writing this blog, have an overarching theme of protecting those in a highly vulnerable setting from adverse outcomes associated with inappropriate antibiotic prescribing. These goals are a great example of nonmaleficence, or the principle to do no harm. Fortunately, as future nurse prescribers we will play a large role in implementing policies such as those mentioned in order to prevent this issue from reaching our patients, and therefore maintaining our ethical obligations.
Christina
Reference:
CDC. (2017). The core elements of antibiotic stewardship for nursing homes. Retrieved from https://www.cdc.gov/longtermcare/prevention/antibiotic-stewardship.html
LikeLike