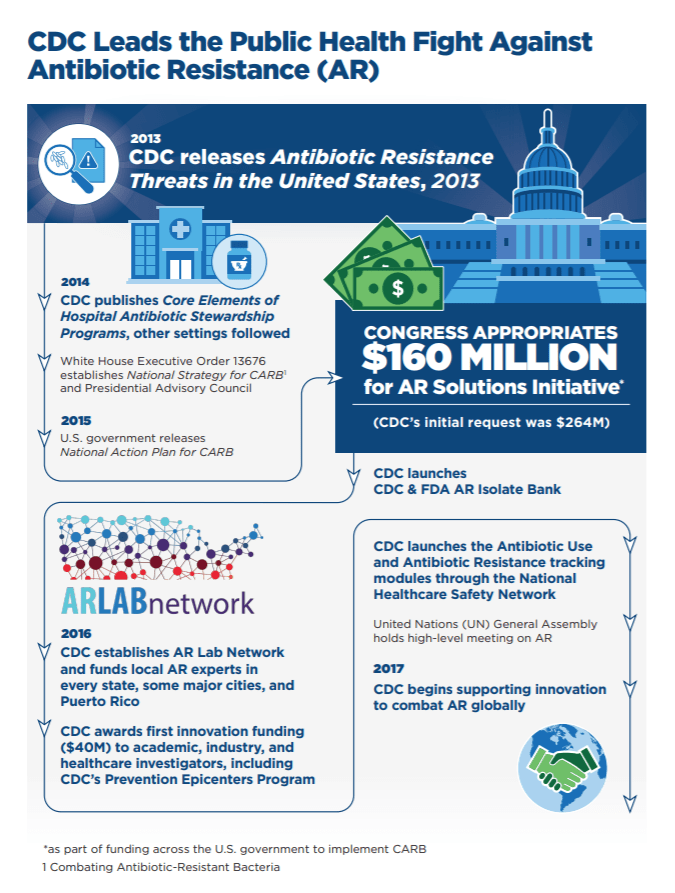
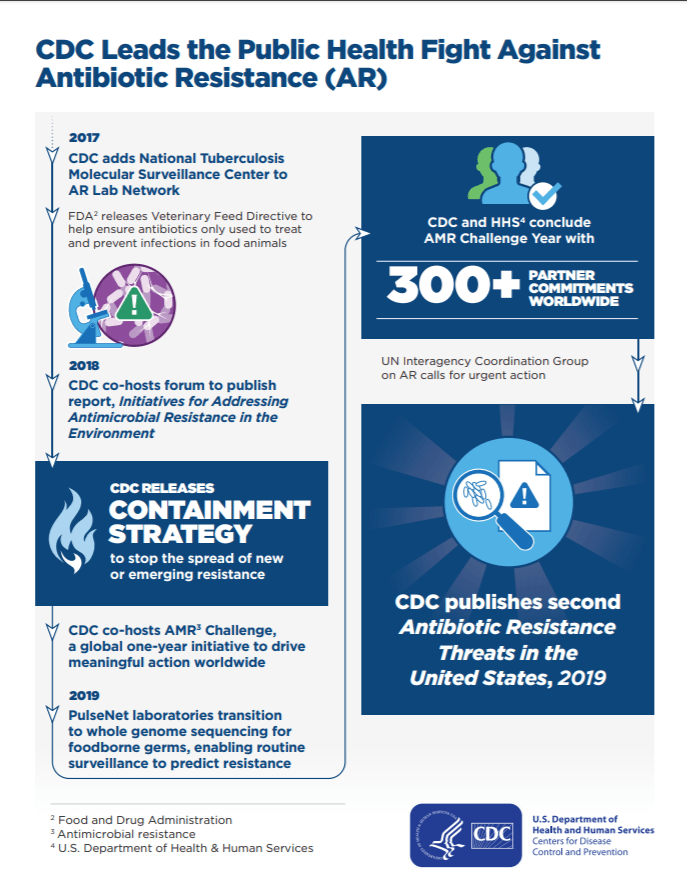
Legislation is a solution to promote a certain policy but may occur over time due to its complex process. As soon as the policy agenda is set judicially and the problem may be clearly identified, a sequence of well-documented stages in which a bill can become a law in both state and federal legislation. Then again, once a bill is introduced, it might never become a law. During 2011 through 2013, in the 112th Congress, only 2% of proposed bills (284) were passed into law. Therefore, being aware of the progress of legislation is important to influence the development of a bill like attending public hearings and reaching out to committees (Paton, Zalon & Ludwick, 2014). The United States government has been addressing antibiotic resistance as a national priority, thus, creating strategies to combat antibiotic overuse and misuse (Centers for Disease Control and Prevention, 2019).
History of Antibiotics Resistance and Stewardship
Alexander Fleming discovered Penicillin in 1928 and emphasized that overuse may diminish its efficacy (Gregory, Suleyman & Barnes, 2018). Since then, the concept of Antibiotic Resistance has been acknowledged and the need for Antibiotic Stewardship has been promoted. As a result of overuse and misuse of antibiotics, microorganisms such as bacteria and viruses generate ways to endure new antibiotics making it hard for healthcare organizations and pharmacies to keep up. Consequently, many infectious disease professional organizations have supported plans to eradicate this threat.
Center for Disease Control and Prevention
In 2009, the CDC started the first didactic attempt to encourage improved antibiotic use in acute-care hospitals (Gregory, Suleyman & Barnes, 2018).
Joint Commission
On June 2, 2015, The Joint Commission (2016) participated in the White House Forum on Antibiotic Stewardship. Later, the Joint Commission established the antimicrobial stewardship criterion for hospitals, critical access hospitals, nursing care centers, ambulatory care organizations, and office-based surgery practices and did a field review in November and December 2015. Subsequently, the Joint Commission announced a new Medication Management standard 09.01.01 addressing that all hospitals, critical access hospitals, and nursing care centers implement Antimicrobial Stewardship effective January 1, 2017.
Centers for Medicare & Medicaid Services (CMS)
CMS encouraged the importance of antibiotic stewardship programs across a variety of clinical practice areas. Therefore, the creation of federal regulations § 482.42(b) and § 485.640(b) that Antibiotic Stewardship programs must be implemented by March 30, 2020.
Collectively, federal organizations are working together to (CDC, 2019):
Respond to new and ongoing public health threats
Strengthen detection of resistance
Enhance efforts to slow the emergence and spread of resistance
Improve antibiotic use and reporting
Advance development of rapid diagnostics
Enhance infection control measures
Accelerate research on new antibiotics and antibiotic alternatives
As healthcare advocates, our role and involvement to healthcare policymaking can be endless. Our voice and engagement with stakeholders may impact the safety of the society especially in issues like Antibiotic Resistance. Although, there is no specific law that demands the need for Antibiotic Stewardship or any punishment if not followed, it is our duty to strengthen our voice as an advocate for all.
References
Centers for Disease Control and Prevention. (2019). U.S. action to combat antibiotic resistance. Retrieved from https://www.cdc.gov/drugresistance/us-activities.html
Gregory, J. R., Suleyman, S. & Barnes, M. N. (2018). A review of the opportunities and shortcomings of Antibiotic Stewardship. Retrieved from https://www.uspharmacist.com/article/a-review-of-the-opportunities-and-shortcomings-of-antibiotic-stewardship
Patton, R. M., Zalon, M. L., & Ludwick, R. (Eds.). (2014). Nurses making policy: From bedside to boardroom. Retrieved from https://ebookcentral-proquest-com.ezproxy1.lib.asu.edu
The Joint Commission. (2016). Approved: New Antimicrobial Stewardship Standard. Retrieved from https://www.jointcommission.org/-/media/enterprise/tjc/imported-resource-assets/documents/new_antimicrobial_stewardship_standardpdf.pdf?db=web&hash=69307456CCE435B134854392C7FA7D76
I found an interesting article that discusses the social norms of antibiotic prescribing from the provider viewpoint. In this article it illuminates the need for more public education about antibiotics in order for providers in all settings, particularly outpatient clinics to have more antibiotic stewardship within their practice. In England, providers that were prescribing 80% greater amount of antibiotics compared to their counterparts were mailed a letter stating that their practice was prescribing antibiotics at a rate much higher than others. These physicians were given information on delaying antibiotics and support for self-care as an initial intervention (Gould and Lawes, 2016). Alerting physicians to a higher rate of prescribing than others in the community is a way to demonstrate that prescriptions are no longer first line intervention for certain illnesses. If there continue to be physicians that prescribe at high rates, it will become increasingly difficult for other providers to retain their patients if there is a provider in the area that is willing to continue to prescribe antibiotics regardless of need. According to this study 28% of physicians are still writing prescriptions when their need is not necessarily warranted (Gould and Lawes, 2016). This stems from the social norm that patient experience is rated higher for a physician that prescribe medications over the recommendation of over the counter treatment and self-care management prior to antibiotics (Gould and Lawes, 2016). Patients tend to see their provider with the hope that an antibiotic will be prescribed to shorten the presenting symptoms and if they leave the visit empty handed, it appears to the patient that the provider did not provide the service expected. It is important to educate the public about why antibiotics are not recommended for every presenting symptom. Social norms must align with the expectations of medicine and policy and in order for providers to have antibiotic stewardship, they must feel comfortable that their patients will not leave for another clinic or provider that will write that prescription. Ensuring all providers are on the same page will certainly aid in a reduction of unnecessary antibiotic prescribing. In the future if legislation allows, the physicians that are prescribing 80% more than other physicians may begin to see financial penalties just like hospitals are penalized for high 30-day readmission rates in order to ensure certain quality indicators are met. Is that what US legislation is attempting in enact at this point? Any sort of punitive rules that are being looked into as a potential future way to combat the social norms of over prescribing?
References
Gould, I.M., & Lawes, T. (2016). Antibiotic stewardship: prescribing social norms. The Lancet 387(10029), 1699-1701. doi: 10.1016/S0140-6736(16)00007-6
LikeLike
There are more than one million elderly people adults in approximately 15,700 nursing homes each year (Stone, Herzig, Agarwal, Pogorzelska-Maziarz, & Dick, 2018). These elderly adults are more susceptible to infection due to several factors including nutrition, dehydration, functional status, incontinence, skin breakdown, immunosuppression, and comorbidities. The estimated prevalence of infections in nursing home residents is roughly two million annually (Stone et al., 2018). There are several contributing factors that increase antibiotic rates in elderly adults residing in nursing homes. The symptomology of infections presents much different in elderly adults than younger adults. Infections can be more difficult to treat and need to be treated quicker in elderly adults.
With all the challenges treating, diagnosing, and managing infections in elderly adults living in nursing homes, to no surprise antibiotic use can easily be misused. Between 47% and 79% of nursing home residents receive antibiotics each year (Stone et al., 2018). Although there is limited national antibiotics stewardship policies, Centers for Medicare and Medicaid Services (CMS) and Center for Disease Control and Prevention (CDC) both have antibiotic stewardship programs to help address this growing issues.
Reference
Stone, P., Herzig, C., Agarwal, M., Pogorzelska-Maziarz, M., & Dick, A. (2018). Nursing Home Infection Control Program Characteristics, CMS Citations, and Implementation of Antibiotic Stewardship Policies: A National Study. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 55. doi.10.1177%2F0046958018778636
LikeLike