Antibiotic Resistance:
A National Priority
Working as a nurse, I have seen how providers have ordered antibiotics unnecessarily. I have worked in a country where pharmacies do not require consumers to have a prescription for antibiotics, do if someone gets sick, people will automatically go to the pharmacy and self-medicate themselves with these medications. I have worked with doctors where common colds can be “cured” by antibiotics. Having these perceptions that “Antibiotics can treatment everything” had stemmed from the discovery of Penicillin in 1928 by Alexander Fleming (Centers for Disease Control and Prevention (CDC), 2019) and our reliance to antibiotics has taken its toll. Unnecessary antibiotic administration has led to increasing incidences of infections that are resistant to antibiotics, making it harder and sometimes impossible to treat (World Health Organization (WHO), 2018). Since antibiotic resistance may affect the healthcare, veterinary and agricultural industries, it is one of the most serious public health problems globally. There is an estimated 2.8 million people in the U.S. have antibiotic resistant infection and more than 35,000 die from it (CDC, 2019).

Antibiotics is one of the most commonly prescribed medications in long term care facilities making it dangerous for the frail residents if administered inappropriately. According to the CDC (2015), 70% of the residents residing in nursing homes get one or more courses of systemic antibiotics in a year but 40-75% of antibiotics prescribed were unwarranted or inappropriate. As a result, the risk for Clostridium difficile, heightened adverse drug outcomes and drug interactions, and colonization and/or infection with antibiotic-resistant organisms may occur in this population (CDC, 2015; WHO, 2018). Since nursing home residents are at high risk of acquiring infection due to immunosuppression, functional and cognitive impairment, the inability to convey symptoms may lead to assumptions in antibiotic prescribing (Van Buul et al. (2015). Therefore, healthcare organizations were forced to create and implement methods to eliminate this problem.
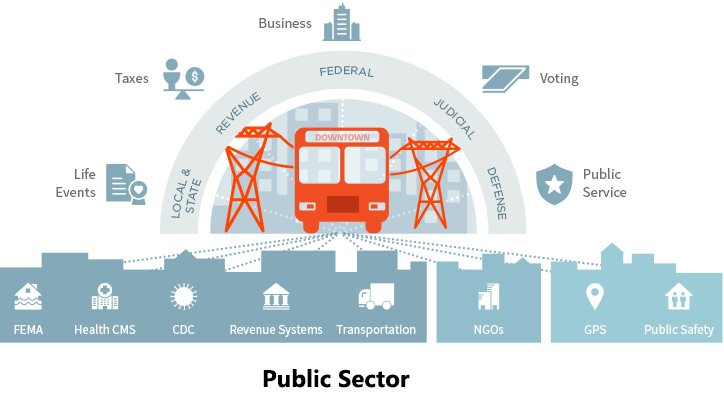
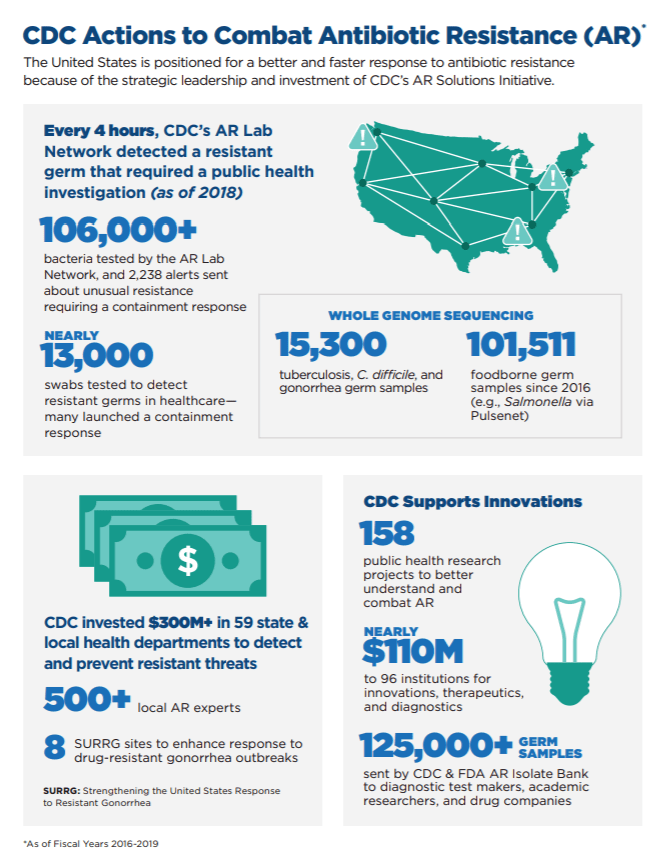
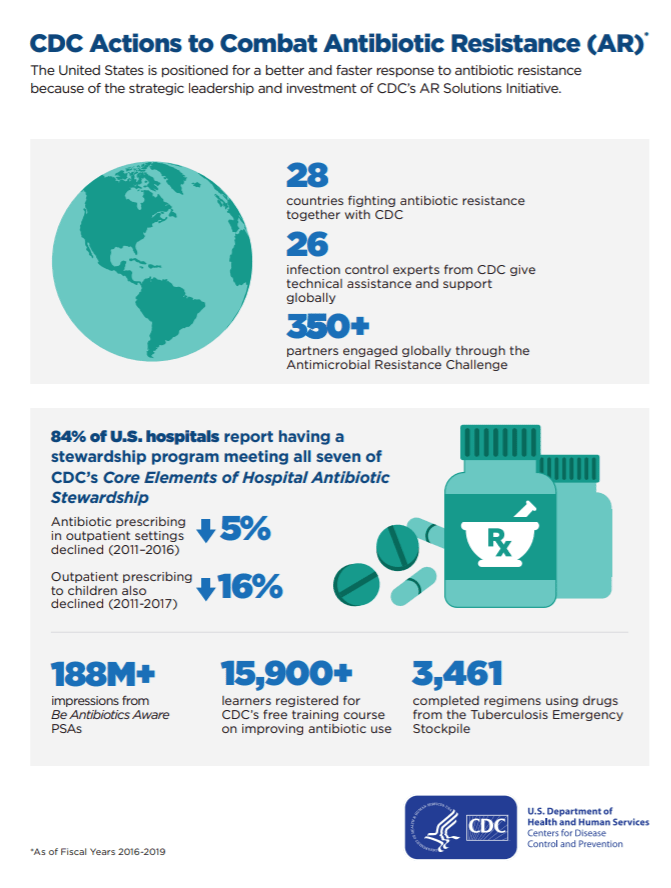
The United States government has been determined to eliminate antibiotic resistance, deeming it as a national priority. Mandates such as U.S. National Strategy for Combating Antibiotic-Resistant Bacteria (National Strategy) and a supplementary U.S. National Action Plan for Combating Antibiotic-Resistant Bacteria (National Action Plan) were implemented to promote Antibiotic Stewardship in all sectors like healthcare, veterinary and agricultural industries. According to the CDC (2019), federal organizations are working together to:
- Respond to new and ongoing public health threats
- Strengthen detection of resistance
- Enhance efforts to slow the emergence and spread of resistance
- Improve antibiotic use and reporting
- Advance development of rapid diagnostics
- Enhance infection control measures
- Accelerate research on new antibiotics and antibiotic alternatives
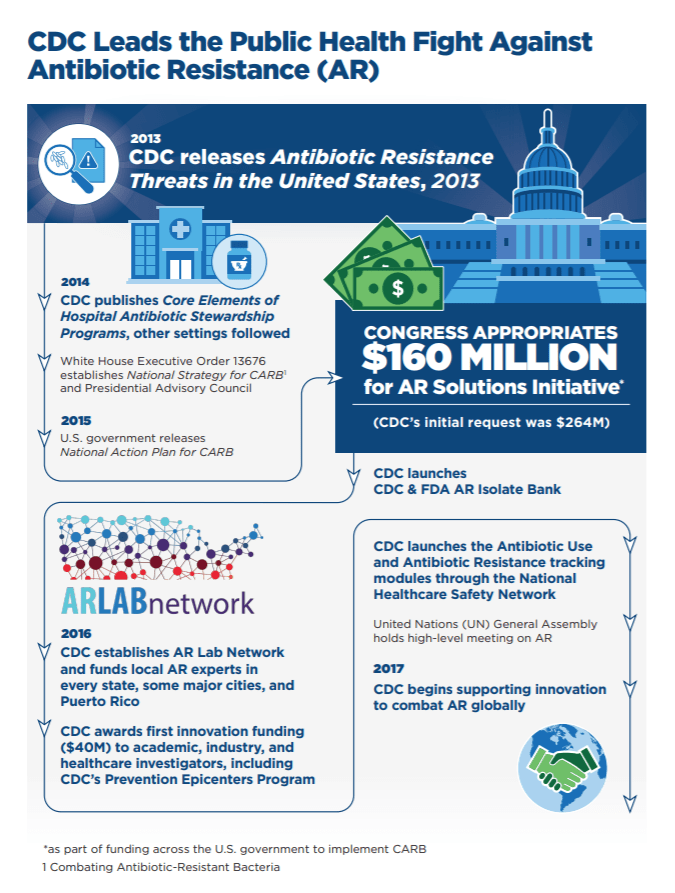
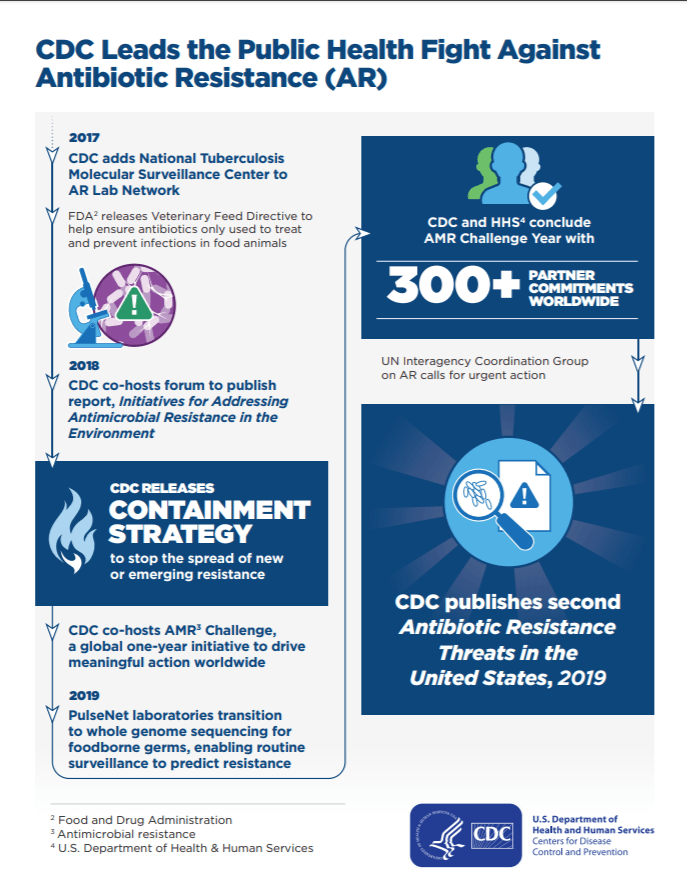
Here is a link of the timeline of the actions done by the government to fight antibiotic resistance: https://www.cdc.gov/drugresistance/pdf/threats-report/CDC-Leads-AR-Fight-508.pdf
In addition, the United Nations (2016) acknowledged that the best practice for managing infections is improved awareness on Antibiotic Resistance. In 2016, the U.S. Congress granted $160 million to the CDC to execute Antibiotic Resistance Solutions Initiative and promote Antibiotic Stewardship (CDC, 2018). The Center for Medicare and Medicaid Services (2018) included the provision of Antibiotic stewardship programs as part of their Long term care facility requirements to practice safe healthcare delivery effective on 2016. Also, the CDC (2016) advocates the implementation of an antibiotic stewardship program following the seven core elements and that all nursing homes develop better antibiotic prescribing practices and decrease unnecessary prescription. Here is the link for the Core Elements of Antibiotic Stewardship for Nursing Homes: https://www.cdc.gov/longtermcare/pdfs/core-elements-antibiotic-stewardship.pdf
In Arizona, the Arizona Department of Health Services (AZDHS) has put into effect a Healthcare Associated Infection (HAI) Advisory Committee to create potential roles and activities to improve antibiotic use in the state like antibiotic stewardship. This involves surveillance, research, creating metrics for measuring advancement towards meeting the national goals and ongoing communication and partnerships with other organizations like Arizona Infectious Disease Society, Arizona Hospital and Healthcare Association and the Arizona Pharmacy Association (AZDHS, 2016).
Executing Antibiotic Stewardship programs in nursing homes can be tough due to inadequate resources. However, through the help of the government and the support of all healthcare professionals, strategic approaches can be applied with minimal expense and effort. Following a stepwise tool for easy understanding, allocating roles, repeated reminders of Antibiotic Stewardship essentials, success will be attained.
References
Arizona Department of Health Services. (2016). Healthcare-associated infection (HAI) & Antibiotic resistance. Retrieved from https://azdhs.gov/preparedness/epidemiology-disease-control/healthcare-associated-infection/index.php#plan
Centers for Disease Control and Prevention. (2015). The core elements of antibiotic stewardship for nursing homes. Atlanta, GA: US Department of Health and Human Services
Centers for disease control and prevention. (2017). Antibiotic use in the United States, 2017: Progress and opportunities. Retrieved from https://www-cdc-gov.ezproxy1.lib.asu.edu/antibiotic-use/stewardship-report/pdf/stewardship-report.pdf
Center for Disease Control and Prevention. (2019). About antibiotic resistance. Retrieved from https://www.cdc.gov/drugresistance/about.html
Center for Disease Control and Prevention. (2019). U.S. action to combat antibiotic resistance. Retrieved from https://www.cdc.gov/drugresistance/us-activities.html
Centers for Medicare and Medicaid Services. (2018). Medicare and Medicaid programs; reform of requirements for long-term care facilities. Retrieved from https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/GuidanceforLawsAndRegulations/Nursing-Homes.html
United Nations. (2016). Draft political declaration of the high-level meeting of the general assembly on antimicrobial resistance. Retrieved from https://www.un.org/pga/71/wp-content/uploads/sites/40/2016/09/DGACM_GAEAD_ESCAB-AMR-Draft-Political-Declaration-1616108E.pdf
Van Buul, L., Van der Steen, J., Achterberg, W., Schellevis, F., Essink, R., De Greeff, S . . . Hertogh, C. (2015). Effect of tailored antibiotic stewardship programmes on the appropriateness of antibiotic prescribing in nursing homes. The Journal of Antimicrobial Chemotherapy, 70(7), 2153-2162. doi: 10.1093/jac/dkv051
World Health Organization. (2018). Antibiotic resistance.Retrieved from https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance